Izpisúa, one step closer to curing diabetes
A team of scientists led by Juan Carlos Izpisúa, director of the Gene Expression Laboratory at Salk Institute in the USA and Extraordinary Professor of Developmental Biology at UCAM, has developed a method, with unprecedented efficiency, that makes it possible to obtain pancreatic β-cells suitable for autotransplantation from human iPS cells.
Diabetes is a chronic disease that occurs when the pancreas does not produce enough insulin (type 1 diabetes) or when the body does not effectively use the insulin it produces (type 2 diabetes). The effect it causes is hyperglycaemia (high blood glucose), which over time seriously damages organs and systems such as the heart, blood vessels, eyes, kidneys or nerves. Currently, more than 400 million people suffer from this disease.
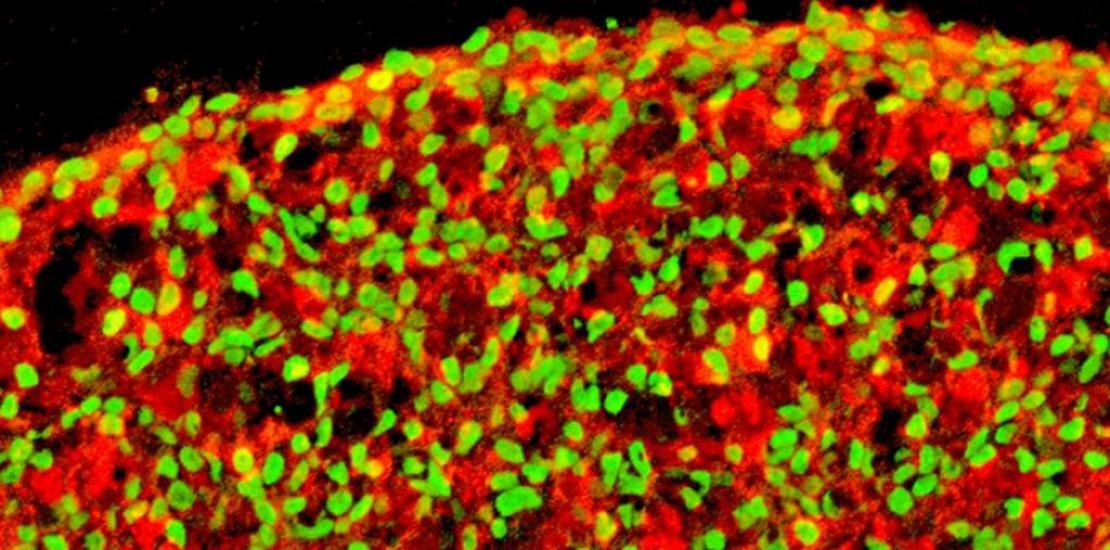
Through this project, promoted and financed by UCAM, with the collaboration of Fundación Primafrío, the team of researchers led by Dr Izpisúa Belmonte has managed to make functional pancreatic β-cells from induced pluripotent human cells (from adult cells). The protocol designed for this has shown unprecedented efficiency from adult cells. “This discovery represents a step forward both for a better understanding of the disease and for its possible treatment”, highlights Dr Izpisúa, principal investigator of the project.
“In vitro and in vivo tests showed that the pancreatic β-cells thus obtained are physiologically functional, that is, they detect glucose and reverse hyperglycaemia in experimental diabetic models in the laboratory. Furthermore, these β-cells, once they are transplanted, are safe and did not form teratomas in the long term”, says Haisong Liu, first author of the work.
Although significant efforts have been made over the past decade to differentiate human iPS cells in pancreatic β-cells, the application of these methodologies in the clinic has been hindered for different reasons: the protocols designed had a low efficiency (~ 10% -40%); the β-cells obtained were very heterogeneous, a high percentage of them lacked the desired functionality and presented a risk of forming teratomas; and the protocols used were highly dependent on the starting cell line, presenting limited value for generating patient-specific β-cells. “All these problems could be due to the lack of knowledge, until now, of how to regulate the signals involved in the transformation of human iPS cells into pancreatic β-cells”, states Llanos Martínez, teacher at UCAM and co-author of the project.
However, in this project, whose results are published in the journal Nature Communications, “we carried out a systematic selection of chemicals and proteins to use in each step of the conversion of human iPS cells into pancreatic β-cells, for which we developed a new protocol”, points out Estrella Núñez, vice-chancellor for Research at UCAM. The designed method is precise and highly efficient for generating pancreatic progenitors from human iPS cells and efficiently grouping them into three-dimensional structures.